ANKLE ARTHRITIS TREATMENT – MELBOURNE
YOUR ANKLE JOINT
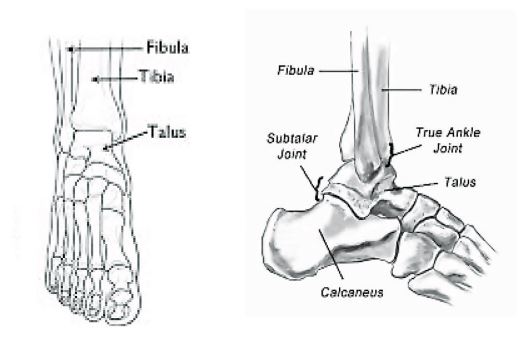
The ankle joint is a hinge joint that connects your foot to your lower leg. The ankle joint is where your shin bone (tibia), calf bone (fibula) and talus bone meet. It allows up and down movement.
Below the ankle is the subtalar joint (the “under ankle” joint). The subtalar joint, between the talus and heel bone (calcaneus) allows side to side movement when you walk on uneven ground.
Your ankle also contains cartilage, ligaments, muscles, nerves and blood vessels. Your ankle has to bear 5 to 7 times your body weight during daily activities, such as standing and walking.
WHAT ARE THE SYMPTOMS OF ANKLE ARTHRITIS?
Pain – Ankle pain is the most common symptom and is usually made worse by walking.
Joint stiffness – With osteoarthritis, ankle joint stiffness or reduced movement is common. With rheumatoid arthritis, also called inflammatory arthritis, stiffness often is worse first thing in the morning.
Cracking/popping/locking – There may be little pieces of loose cartilage or bone caught within the joint causing this sensation.
Ankle weakness or giving way – This may be due to looseness of the ligaments, or secondary due to to pain.
Swelling – Swelling may be as a result of extra bone, or fluid within the joint. The soft tissues around your ankle can also inflame and swell.

ANKLE ARTHRITIS – NON-OPERATIVE TREATMENTS
Modifying the way, you lead your life should be tried first. This may include:
Check with your general practitioner or pharmacist that NSAID’s are suitable for you, as they may have side effects, especially if you have asthma, or stomach ulcers.
For many people pain from arthritis can be eased through using an ankle brace and or a high topped, lace up walking boot with a cushioned sole. Elasticized boots commonly don’t provide a great amount of support.
Dietary supplementation with Chondroitin and Glucosamine, which can be bought in health food shops, may be effective in some patents with early symptoms of ankle arthritis. Hydrotherapy can be very helpful with pain and stiffness.
Patents with inflammatory arthritis are usually looked after by a Rheumatologist. Disease modifying ant-rheumatoid drugs (DMARD’s) are used to treat these conditions, in conjunction with painkillers and NSAID’s.
ANKLE ARTHRITIS – OPERATIVE TREATMENTS
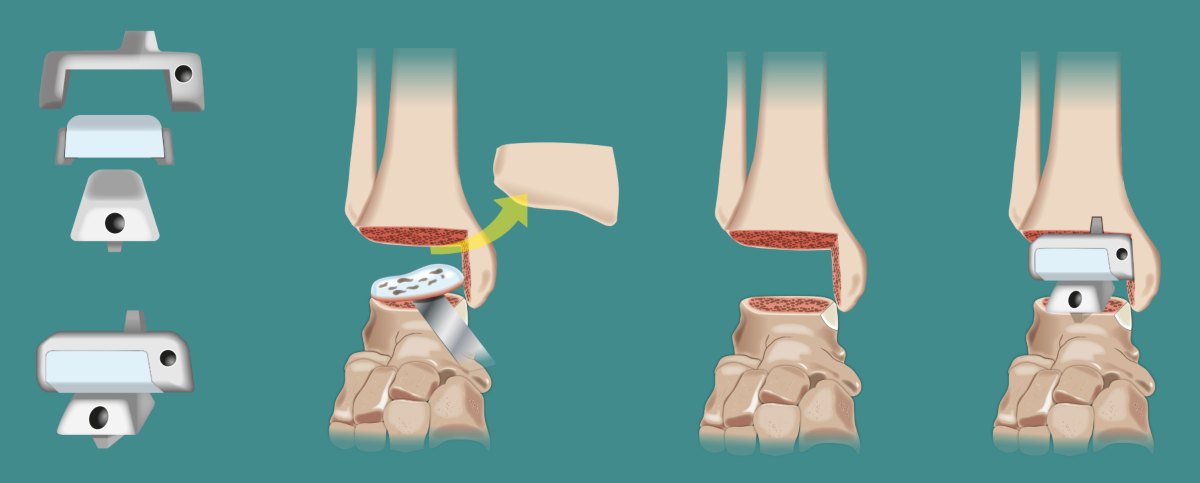
Operative treatments for ankle arthritis include, arthroscopic debridement, ankle joint fusion and total ankle replacement. Access the buttons below to find out more:
POST-OPERATIVE CARE
After ankle joint fusion or a total ankle replacement operation you will go into a plaster splint and remain non weight bearing until your 2 week review with Mr Keith. You will then have a below knee cast fitted and allowed to commence weight bearing in the cast. A repeat x-ray is taken at your 6 and 12 week reviews to confirm the joint is fusing. The plaster cast is finally removed at 12 weeks and you are able to weight bear as tolerated.
Following removal of the cast, a compression or flight sock maybe helpful to reduce swelling. It will be at least 6 months until the benefits of surgery become apparent.
In the longer term, walking and golf are possible, but only the occasional person will be able to jog. You may walk with a limp, but this is usually less marked than it was before surgery, as a result of the reduced pain.
Following surgery, there will be limitation of the height of the heel that you can wear (usually less than 3cm). Some will find wearing a shoe with a curved “rocker bottom” sole will help walking.

A Message from Mr Keith
These guidelines are intended to help you understand your treatment and prepare for your operation.
I understand the level of detail may cause concern or worry for some patients.
If you do have further questions, please don’t hesitate to ask me at your consultation or contact a member of my team.
We will happily address your concerns.
It is important for me that you feel comfortable and satisfied you have all the information you need before your surgery day.
Mr Troy Keith – Orthopaedic Foot & Ankle Surgeon.
Any questions please email
Ankle Arthritis Treatment Melbourne
Mr Keith sees patients from all over Melbourne to diagnose and treat ankle arthritis. Mr Keith consults with patients from the following practice locations in Melbourne including Armadale, Heildelberg and Shepparton in country Victoria.